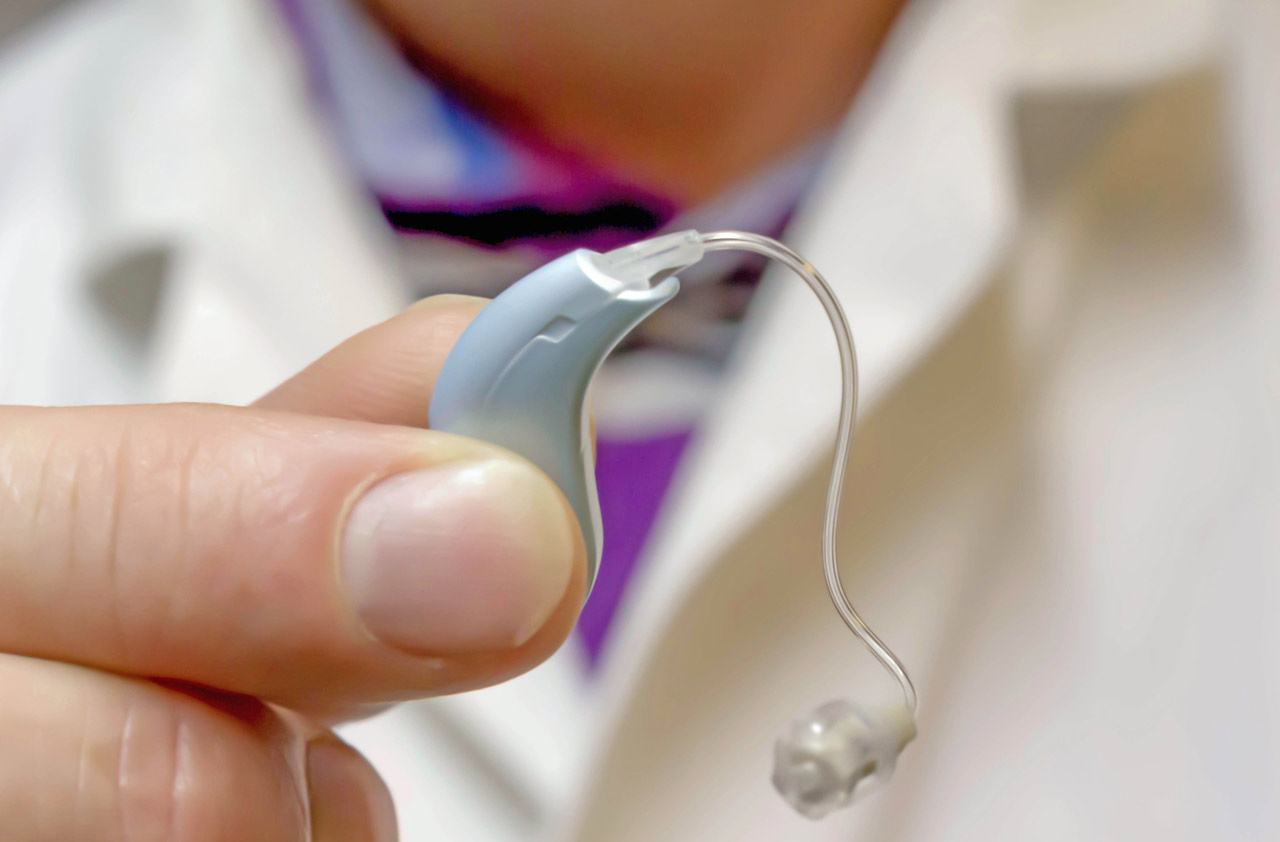
Hearing loss affects millions of people worldwide, yet hearing aids—essential devices that significantly improve quality of life—are often not covered by health insurance. This frustrating gap in coverage leaves many individuals, especially seniors, struggling to afford the devices they need to stay connected, independent, and mentally sharp.
The question is clear: Why are hearing aids not covered by insurance?
The answer lies in a complex web of historical classification, cost structures, policy limitations, and perceptions about hearing loss. Here's a detailed breakdown of why this essential medical need is frequently excluded from standard health insurance plans.
1. Hearing Aids Are Classified as “Elective” or “Non-Essential”
One of the primary reasons hearing aids aren’t covered by insurance is their classification as elective or non-essential devices. Unlike pacemakers or insulin, hearing aids are often considered "lifestyle improvements" rather than critical medical necessities.
Insurers typically reserve coverage for treatments that are:
Life-saving
Emergency-based
Surgically necessary
Prescribed for acute conditions
Because hearing loss is typically gradual, non-life-threatening, and more associated with aging, insurers do not categorize hearing aids in the same tier as other medical treatments. This outdated classification is one of the biggest barriers to coverage.
2. Medicare’s Historical Exclusion Sets the Standard
In the United States, Medicare plays a major role in influencing what private insurers cover. When Medicare was established in 1965, it explicitly excluded hearing aids from coverage, labeling them as devices that “are routinely needed and low in cost.”
At the time, hearing aids were relatively inexpensive and not as technologically advanced. However, decades later, even though hearing aids have become sophisticated and expensive, the exclusion remains.
Because Medicare doesn’t cover hearing aids, many private insurance plans follow suit, especially those modeled after or integrated with Medicare Advantage programs.
3. Cost Control and Risk Pool Management
From an insurer’s point of view, covering hearing aids could be very costly:
Hearing aids typically cost between $2,000 to $7,000 per pair.
Most people with hearing loss need new devices every 3–5 years.
Hearing loss is common with aging, meaning a large portion of the insured population could qualify.
If insurance companies were to include full hearing aid coverage in all standard plans, it would significantly increase premiums for everyone. In response, insurers often choose to exclude these devices altogether or provide limited benefits (such as a small allowance every few years).
4. Fragmented Regulation and Lack of Mandates
Unlike coverage for prenatal care or vaccinations, there is no universal mandate requiring insurers to cover hearing aids. Coverage often varies by:
State (in the U.S.)
Type of plan (employer-sponsored vs. individual)
Age group (children vs. adults)
For example:
Some states require insurers to cover hearing aids for children, but not for adults.
Some employer-sponsored health plans include discount programs or partial reimbursement, but few offer full coverage.
Medicaid may offer hearing aid benefits depending on the state, but eligibility and limitations vary widely.
This lack of federal or global standardization makes access to hearing aids highly inconsistent and inequitable.
5. Perception of Hearing Loss as a Normal Part of Aging
Hearing loss is often seen as a natural consequence of getting older—much like gray hair or wrinkles. This perception leads to the assumption that it’s something people should simply cope with, rather than treat medically.
But that’s not true.
Untreated hearing loss has been linked to cognitive decline, social isolation, depression, and falls.
Research shows that hearing aids can significantly improve mental acuity, communication, and quality of life.
Despite this, the prevailing belief that hearing aids are a “personal responsibility” rather than a “medical necessity” continues to influence insurance policy decisions.
6. High Markups and Lack of Price Transparency
Another issue lies in the pricing structure of hearing aids, which can discourage insurers from offering coverage.
Hearing aids are often bundled with testing, fitting, and service fees.
Manufacturers and audiologists may charge steep markups, making it difficult to determine the actual cost of the device.
Unlike prescription drugs, hearing aids are not subject to the same price controls or competitive transparency.
Because the market lacks regulation, prices vary wildly, and insurers often view the industry as difficult to managewithin a coverage model. Without standardization, offering consistent reimbursement becomes a challenge.
7. Emerging OTC Hearing Aids and Market Disruption
In recent years, the U.S. Food and Drug Administration (FDA) has approved over-the-counter (OTC) hearing aids for mild to moderate hearing loss. These devices are significantly cheaper and can be purchased without a prescription.
This has led some insurers to argue that low-cost solutions now exist, reducing the need for traditional coverage. However, OTC hearing aids are not suitable for:
Severe hearing loss
Children or adolescents
Individuals with complex ear conditions
Still, the availability of OTC options has slowed policy reform, as insurers claim consumers have more affordable choices than ever.
8. What Limited Coverage May Be Available
Though comprehensive hearing aid coverage is rare, some insurance plans may offer partial benefits such as:
Annual or biannual allowances (e.g., $500 every 3 years)
Discount programs through audiologist networks
Coverage for diagnostic hearing exams, but not the device
Medicaid coverage in select states or regions
If you or a loved one needs hearing aids, it's important to read your policy carefully, check state laws, and consult with your insurance provider to explore any available options.
9. Advocacy and Reform Are Gaining Momentum
The lack of insurance coverage for hearing aids has come under growing scrutiny. Advocates and medical professionals are pushing for reforms, citing research showing the serious health consequences of untreated hearing loss.
Some key developments include:
The Over-the-Counter Hearing Aid Act, which increases accessibility.
Discussions about adding hearing aid benefits to Medicare in future healthcare reforms.
Pressure on private insurers to cover hearing aids in employer-sponsored plans.
Growing awareness of the connection between hearing health and cognitive function, especially with the rise in Alzheimer’s and dementia concerns.
While change is slow, public health pressure is building. Future insurance models may better reflect the essential nature of hearing care.
Conclusion: Why Hearing Aids Remain Largely Uncovered
Despite their critical role in improving communication, mental health, and daily life, hearing aids continue to be excluded from most health insurance plans. The reasons stem from outdated classifications, high costs, lack of legal mandates, and perceptions that hearing loss is simply part of growing older.
Until regulations shift and awareness grows, individuals are left to pay out-of-pocket, use limited discount programs, or explore over-the-counter solutions. If you're affected by this gap in coverage, consider advocating for change—through your employer, local legislature, or national health organizations.
As the population ages and the link between hearing and brain health becomes more widely accepted, there is hope that hearing aids will one day be treated—and covered—like the essential medical devices they truly are.